When it comes to a healthcare practice’s finances, the duties of medical billing and coding experts are indispensable. They ensure that all claims and supporting documents are properly coded for swift and hassle-free reimbursements. But aside from crunching the numbers, there is a lot more that goes into these roles to ensure efficiency in revenue cycle management (RCM).
In this post, we’ll give you a quick breakdown of the difference between medical billing and coding and why they are extremely crucial in healthcare.
What is medical billing?
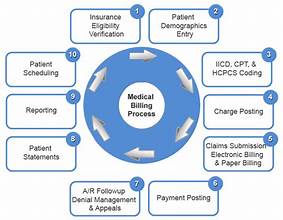
Understanding the importance of medical billing in the RCM can help you grasp its entire process.
In general, medical billing involves the submission and processing of claims for medical services rendered by healthcare providers. These are submitted to insurance companies, payers, or patients directly. This means that billers are responsible for strategies for medical bill collections.
For this part, medical billers ensure that healthcare providers receive timely reimbursement for their services. This way, practices can sustain their operations and continue delivering quality care.
Moreover, medical billers review medical documentation like patient records, treatment plans, and diagnosis codes. Their job is to ensure its accuracy before filing a detailed claim. This way, they can prevent denials, rejections, or any delays in payments.
What is medical coding?
Understanding medical billing & coding also involves getting to know what the latter’s unique role is.
While medical billing focuses on creating claims for reimbursement, medical coding translates medical procedures, diagnoses, and treatments into universally recognized alphanumeric codes. These codes serve as a standardized language between healthcare providers, insurance companies, and regulatory bodies.
For this, coders use two primary coding systems: the International Classification of Diseases (ICD) and the Current Procedural Terminology (CPT). The ICD codes categorize diagnoses and diseases, while CPT codes outline specific medical procedures and services.
Overall, medical coding requires precision and in-depth medical knowledge. They also need to be certified before handling medical bill collections roles.
The role of medical billing and coding in revenue cycle management
Together, medical billing and coding ensure that a practice’s revenue cycle will be streamlined and error-free. This includes taking the following responsibilities:
1. Patient Registration
Before any medical services can be billed or coded, billers will register patients within the healthcare organization’s system. This step involves capturing personal information, insurance details, and establishing financial responsibility agreements.
2. Documentation and Coding
Once a patient receives medical services, healthcare professionals document all necessary information. This includes details about the diagnosis, treatment provided, medications administered, and any additional procedures performed. From there, medical coders review these documents and assign appropriate codes.
3. Claims Submission
After the medical coding process is complete, medical billers compile the necessary information to file the claims. These claims contain all relevant details about the services provided, including the corresponding codes, costs, and any supporting documentation.
From there, medical billers will submit these claims electronically to insurance companies or patients themselves. Timely submission is important to avoid payment delays.
4. Claims Adjudication
Upon receiving the claims, insurance companies review them to determine their eligibility for payment. This process is known as claims adjudication.
During adjudication, insurance companies assess whether the services match with the coverage on the patient’s insurance plan. They also verify if the assigned codes are accurate and if they meet specific criteria for reimbursement.
5. Payment Posting and Reconciliation
Once a claim is approved, medical billers are responsible for posting the payment to the patient’s account within the healthcare organization’s system. This highlights the impact of medical bill collections within the revenue cycle.
This step involves reconciling the payment with the original claim amount. During this process, billers may perform adjustments or write-offs.
Benefits of revenue cycle management services
Dealing with medical bill collections and claims processing is often an overwhelming task for doctors and their organizations. This is why they prefer to partner with revenue cycle management services to handle the financial aspect of their industry.
With this, healthcare organizations and practices enjoy the following benefits from professional RCM services:
Increases revenue collection for a steady cash flow
Reducing the risk of claim denials/rejections due to errors
Ensuring regulatory compliance to avoid penalties and/or sanctions
Streamlining the practice’s operations through effective financial processes
Allowing medical practitioners to provide better patient care without worrying about their revenue collections
Keeping the cash flow predictable allows healthcare organizations to expand their practice.
Reducing administrative burdens, especially for small practices with limited in-house resources.
Conclusion
Medical billing and coding are two of the most important segments of revenue cycle management. If done right, it can help boost the financial health of any medical practice.
Also, the importance of revenue cycle management isn’t only about the organization’s benefit. It also trickles down to the patients and the quality of care they will receive. Overall, it’s a win-win situation for healthcare professionals, patients, medical billers, and medical coders.


 Home
Home