The Telltale Visual Signs
Shoulder injuries can be alarming. Our shoulder is the most flexible joint in the body. This also makes it the most commonly dislocated joint. When a shoulder pops out of place, it needs immediate attention.
Understanding what a dislocated shoulder looks like is crucial for prompt action. It can prevent more serious damage.
In this comprehensive guide, we will walk you through the telltale visual signs. We will also cover the important sensory clues you might experience. This knowledge will help you identify a dislocated shoulder quickly and confidently.
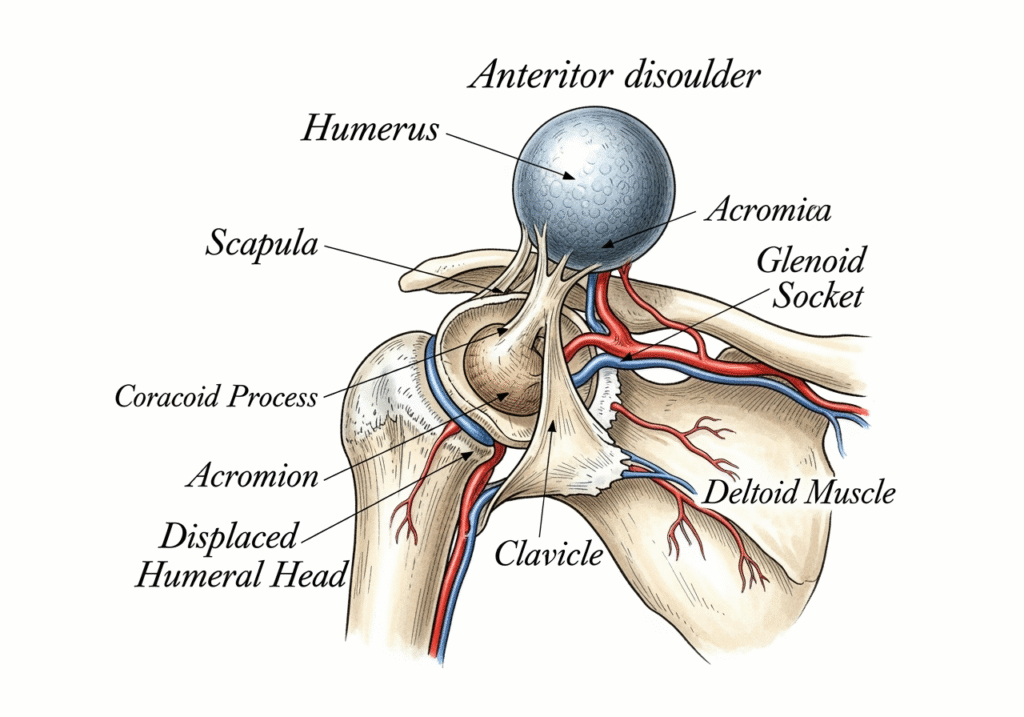
When a shoulder dislocates, the immediate impact is often visible. The normally smooth, rounded contour of the shoulder can undergo a dramatic and unmistakable change. These visual cues are often the first indicators that something is seriously wrong and that the humerus (upper arm bone) has been forced out of its glenoid (shoulder socket). Recognizing these changes is paramount for swift and appropriate action.
A Change in Shoulder Contour
The healthy shoulder typically presents a smooth, rounded contour, primarily due to the underlying deltoid muscle. This muscle drapes over the ball of the humerus, giving the shoulder its characteristic shape. However, in the event of a dislocation, this familiar appearance is immediately altered.
One of the most striking visual signs is a “squared-off” or “flattened” appearance of the shoulder. Instead of the gentle curve, the shoulder may look angular, as if a significant portion of its natural bulk has vanished. This occurs because the humeral head, which normally fills the socket and creates that rounded shape, has moved out of place. When it’s no longer beneath the deltoid, the muscle may appear to sag inward, creating a depression or a “loss of deltoid curve.” This can make the acromion, the bony prominence at the top of the shoulder blade, appear unusually prominent or sharp. There might be a noticeable “sunken area” or hollow directly below the acromion where the humeral head should be. This visual deficit is a strong indicator of a dislocated shoulder.
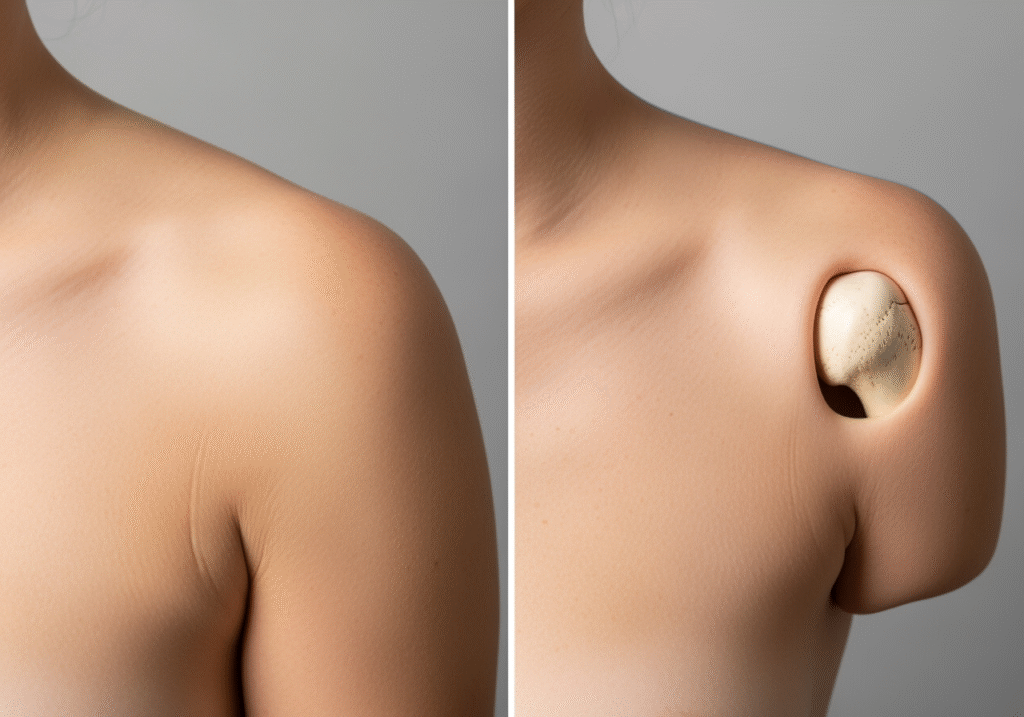
The degree of deformity can vary depending on the direction of the dislocation (which we will discuss later), but a noticeable alteration from the normal symmetrical appearance of the shoulders is almost always present. Comparing the injured shoulder to the uninjured one often reveals a stark contrast, highlighting the severity of the injury. This visible deformity is a critical clue that helps us understand what a dislocated shoulder looks like.
Unnatural Arm Position and Swelling
Beyond the altered contour, the position of the arm itself offers significant clues. A person with a dislocated shoulder will instinctively adopt a protective posture, often holding the injured arm rigidly. This is an involuntary response to minimize pain and prevent further damage. The arm is typically held away from the body, often slightly abducted (moved outward) and externally rotated, making it impossible to bring the arm across the chest or move it in any natural way. Any attempt to move the arm, even slightly, will elicit intense pain. This fixed, unnatural position is a hallmark of a dislocated shoulder and is caused by the humerus being jammed out of alignment and the surrounding muscles going into protective spasm.
Accompanying these visual deformities, you will almost certainly observe swelling and bruising around the affected joint. The immediate trauma of the dislocation causes damage to blood vessels and soft tissues, leading to a rapid accumulation of fluid and blood. Swelling can make the shoulder appear larger than normal, further distorting its shape. Bruising, which may not appear immediately but will develop over hours or days, can range from red and purple to greenish-yellow as the blood components break down. This discoloration can extend down the arm and even onto the chest.
Furthermore, in some cases, you might be able to see or feel a distinct “visible lump or bulge” where the humeral head has displaced. Depending on the direction of the dislocation, this bump might be on the front of the shoulder, beneath the collarbone, or even at the back. This palpable abnormality, combined with the altered contour and unnatural arm position, paints a clear picture of a dislocated shoulder. It’s a testament to the significant displacement that has occurred within the joint.
Feeling the Dislocation: Key Sensory Clues
While visual signs are often the most obvious, the sensory experiences accompanying a dislocated shoulder are equally, if not more, defining. These internal sensations provide critical information about the nature and severity of the injury.
Intense Pain and Immobility
The onset of a shoulder dislocation is almost universally marked by sudden, excruciating, and unrelenting pain. This is not a dull ache or a minor discomfort; it is a sharp, tearing, or grinding sensation that can be profoundly debilitating. The pain is immediate and severe because the dislocation involves the forceful tearing or stretching of ligaments, joint capsules, and other soft tissues that normally hold the joint together. Nerves are also stretched or compressed, contributing to the intense agony.
Following this initial burst of pain, the ability to move the injured joint becomes severely compromised, if not entirely impossible. The arm feels “dead” or completely useless. This immobility is partly due to the mechanical obstruction of the humeral head being out of its socket, but also significantly due to involuntary muscle spasms. The muscles surrounding the shoulder joint, in an attempt to protect the injured area and prevent further movement, contract powerfully and painfully. This “guarding” of the arm is a protective mechanism, but it greatly exacerbates the pain and makes any voluntary movement agonizing.
Many individuals also describe a distinct “popping” or “clunking” sensation at the exact moment of injury. This sound or feeling signifies the humeral head forcefully exiting the glenoid socket. Immediately after, there’s a profound “feeling of instability” – a sensation that the shoulder is no longer securely in place, often accompanied by a deep, aching pain that persists until the joint is reduced. This combination of intense pain, complete immobility, and a feeling of profound instability leaves little doubt about the nature of the injury.
Numbness, Tingling, and Muscle Spasms
Beyond the immediate, sharp pain, a dislocated shoulder can also manifest neurological symptoms due to the stretching or compression of nerves that run through the shoulder and down the arm. It’s common for individuals to experience “numbness down the arm,” often extending into the hand and fingers. This can be accompanied by “tingling” sensations, often described as “pins and needles.” In more severe cases, there might be noticeable “weakness” in the arm, making it difficult to grip objects or perform simple tasks.
The most commonly affected nerve is the axillary nerve, which supplies sensation to a small patch of skin over the outer part of the shoulder (the “regimental badge” area) and controls the deltoid muscle. Damage to this nerve can lead to numbness in that area and weakness in lifting the arm. Other nerves of the brachial plexus, a network of nerves that originates in the neck and extends into the arm, can also be affected, leading to more widespread sensory or motor deficits. These neurological symptoms are a serious concern and highlight the importance of prompt medical evaluation to assess nerve integrity.
As mentioned earlier, “painful muscle spasms” are a significant component of a dislocated shoulder. These involuntary contractions of the shoulder muscles (like the deltoid and rotator cuff) are the body’s attempt to stabilize the unstable joint. However, they also contribute immensely to the pain and make it incredibly difficult for the patient to relax the arm, which is necessary for a successful reduction. The spasms can be so intense that they prevent the shoulder from being put back into place without strong pain medication or muscle relaxants. The combination of these sensory and neurological clues provides a comprehensive understanding of the distress and functional impairment caused by a dislocated shoulder.
What Does a Dislocated Shoulder Look Like Based on Type?
While the general signs of a dislocated shoulder are consistent, the specific visual presentation can vary depending on the direction in which the humeral head displaces. Understanding these distinctions helps in initial assessment, though only a medical professional can provide a definitive diagnosis.
Anterior Dislocation (Most Common)
Anterior dislocations are by far the most prevalent type, accounting for approximately 95% of all shoulder dislocations. In this scenario, the humeral head moves forward and typically comes to rest beneath the coracoid process (a hook-like projection from the shoulder blade) or even further forward.
Visually, an anterior dislocation presents with several distinctive features. The most prominent is the “squared-off” appearance of the shoulder, as the rounded contour of the deltoid muscle is lost. The acromion, the bony tip of the shoulder, will appear very prominent. Crucially, the “humeral head is often palpable in front,” creating a noticeable bulge or lump in the anterior aspect of the shoulder, sometimes described as a “golf ball under the skin.” This lump is the displaced ball of the arm bone.
The arm itself will typically be held in a position of “abduction and external rotation.” This means the arm is moved away from the body and rotated outward, often with the elbow bent and the forearm pointing away from the body. The patient will be unable to bring their arm back to their side or rotate it internally due to pain and mechanical blockage. Conversely, there will be a noticeable “hollow area at the back of the shoulder” where the humeral head normally sits. This combination of a prominent anterior bulge, a squared-off shoulder, and the characteristic arm posture is highly indicative of an anterior dislocation.
Posterior and Inferior Dislocations (Less Common)
While anterior dislocations dominate, it’s important to be aware of the less common, but equally serious, posterior and inferior dislocations. These can be more challenging to diagnose visually, as their deformities may be less obvious.
Posterior Dislocation: This type occurs when the humeral head moves backward, often due to a direct blow to the front of the shoulder, or in cases of seizures or electrocution. Visually, the “arm is typically held in adduction and internal rotation.” This means the arm is held close to the body, rotated inward, and the patient often cannot externally rotate it. The anterior aspect of the shoulder may appear “flattened anteriorly” or even concave, as the humeral head is no longer there. The “prominent coracoid process” might be more noticeable. Sometimes, a posterior bulge can be felt, but it’s often less obvious than the anterior bulge in an anterior dislocation. Because the shoulder may not look as dramatically deformed, posterior dislocations are sometimes missed or misdiagnosed initially.
Inferior Dislocation (Luxatio Erecta): This is the rarest and most severe type of shoulder dislocation. It occurs when the humeral head displaces directly downward, often with such force that the arm remains “stuck overhead,” pointing upwards. The patient cannot bring their arm down to their side. This posture is highly distinctive and almost diagnostic on its own. It’s a medical emergency due to the high risk of neurovascular complications. While rare, its dramatic visual presentation makes it unmistakable once seen.
Understanding these different presentations helps in quickly assessing the injury, but it’s crucial to remember that all suspected dislocations require immediate medical attention for proper diagnosis and reduction.
Immediate Steps for a Suspected Dislocation
When faced with a suspected dislocated shoulder, immediate and appropriate action can significantly impact the outcome, minimize pain, and prevent further injury. While waiting for professional medical help, there are crucial steps to take, and equally important actions to avoid.
What to Do: The R.I.C.E. Principles Modified
Our primary goal is to stabilize the situation and make the individual as comfortable as possible until medical professionals can intervene.
- Seek Immediate Medical Attention: This is the most critical step. A dislocated shoulder is a medical emergency and requires prompt attention. Do not delay. We should transport the individual to the nearest emergency room or call for an ambulance if movement is too painful or difficult. The longer a shoulder remains dislocated, the more difficult it can be to reduce, and the higher the risk of complications such as nerve damage or compromised blood supply.
- Immobilize the Arm: It is vital to prevent any movement of the injured shoulder. We can achieve this by gently supporting the arm in the position it is found. Do not try to move it into a “more comfortable” position if it causes pain. A simple sling, or even a towel or piece of clothing tied around the arm and neck, can provide temporary support and prevent accidental movement. The aim is to keep the arm still and close to the body, minimizing any strain on the dislocated joint. This immobilization helps to reduce pain and prevent further damage to the surrounding tissues, ligaments, and nerves.
- Apply Ice Packs: Once the arm is immobilized, applying ice packs to the affected area can help significantly. We should place a cloth or towel between the ice pack and the skin to prevent frostbite. Apply ice for 15-20 minutes at a time, every few hours. Ice helps to “reduce swelling and pain” by constricting blood vessels and numbing the area. It’s an effective first-aid measure for managing discomfort while awaiting medical care.
These steps are for temporary relief and stabilization only. They are not a substitute for professional medical intervention.
What NOT to Do
Just as important as knowing what to do is understanding what not to do. Attempting to “fix” a dislocated shoulder without proper medical training can lead to severe and irreversible damage.
- Do Not Attempt to Pop It Back In: This is perhaps the most crucial “do not.” We understand the instinct to try and realign the joint, especially if someone has seen it done in movies or has experienced it before. However, attempting “self-reduction” or allowing an untrained person to manipulate the shoulder is extremely dangerous. The humeral head can get caught on nerves, blood vessels, or bone fragments, leading to fractures, nerve damage (which can cause permanent weakness or numbness), or even damage to the blood supply of the arm. Only a trained medical professional, typically in a controlled environment with proper pain management and imaging, should attempt to reduce a dislocated shoulder.
- Do Not Move the Joint Excessively: Any forceful or unnecessary movement of the dislocated joint can worsen the injury. We must avoid trying to test the range of motion or forcing the arm into different positions. This can further tear ligaments, damage the joint capsule, or cause additional fractures. The goal is to keep the arm as still as possible in its current, albeit uncomfortable, position.
- Do Not Eat or Drink: If the individual is likely to require sedation or general anesthesia for the reduction procedure, it’s important that their stomach is empty. Eating or drinking before anesthesia can lead to complications such as aspiration (inhaling stomach contents into the lungs). Therefore, it’s best to refrain from giving the person any food or drink once a dislocation is suspected.
By adhering to these guidelines, we can ensure the safest possible environment for the injured individual until they receive professional medical care.
Frequently Asked Questions about Shoulder Dislocations
When a shoulder dislocates, many questions naturally arise regarding its immediate management, diagnosis, and long-term recovery. Here, we address some of the most common inquiries.
Can a dislocated shoulder fix itself or pop back in on its own?
While rare, a dislocated shoulder can, in very few instances, spontaneously reduce (pop back into place) on its own, often immediately after the injury or with a very slight movement. However, this is the exception, not the rule. For the vast majority of cases, a dislocated shoulder will not fix itself and requires intervention from a medical professional.
Attempting to force it back into place yourself, or having an untrained person try, carries significant risks. As we’ve discussed, this can lead to further injury, such as fractures, or damage to critical structures like nerves and blood vessels. For instance, the axillary nerve, which is vital for shoulder function and sensation, runs very close to the shoulder joint and is vulnerable during forceful, unguided manipulation. The “importance of proper diagnosis” cannot be overstated. A medical professional will first take X-rays to ensure there are no fractures or other complications before attempting reduction. They will also use appropriate pain relief and muscle relaxants to make the process safer and less painful. Therefore, if a shoulder is suspected to be dislocated, seeking immediate medical attention is always the safest course of action.
How is a dislocated shoulder officially diagnosed by a doctor?
The diagnosis of a dislocated shoulder typically begins with a thorough “physical examination.” The doctor will observe the visually apparent deformities, such as the squared-off shoulder and unnatural arm position. They will also gently “checking for deformity and pulses” in the wrist and hand to ensure blood flow is not compromised. “Assessing nerve function” is crucial; this involves checking sensation (e.g., light touch over the deltoid for axillary nerve integrity) and the ability to move fingers and wrist. The doctor will typically ask about the mechanism of injury and the patient’s symptoms.
The definitive diagnosis, however, is confirmed through imaging. “X-rays to confirm dislocation” are standard. These images clearly show the position of the humeral head relative to the glenoid socket. X-rays are also vital to “rule out associated fractures,” as dislocations can sometimes occur concurrently with a broken bone (e.g., a fracture of the humeral head, known as a Hill-Sachs lesion, or a fracture of the glenoid rim, known as a Bankart lesion). In some complex cases, or if there’s suspicion of significant soft tissue damage (like a torn labrum or rotator cuff), an MRI or CT scan might be ordered for a more detailed view. This comprehensive diagnostic approach ensures that the dislocation is properly identified and any accompanying injuries are not missed.
What is the typical recovery process after a shoulder is put back in place?
Once the dislocated shoulder has been successfully reduced (put back into its socket), the recovery process begins, focusing on pain management, healing, and restoring function.
- Immobilization: The shoulder will typically be placed in a sling or shoulder immobilizer for a period, usually ranging from a few days to a few weeks. The duration depends on the individual’s age, the severity of the dislocation, and whether it’s a first-time or recurrent injury. This “immobilization in a sling” allows the stretched or torn ligaments and joint capsule to begin healing.
- Pain Management: “Pain management” is crucial during the initial recovery phase. This involves prescribed pain medications, anti-inflammatory drugs, and continued application of “ice” to reduce swelling and discomfort.
- Physical Therapy: This is a cornerstone of recovery. Once the initial pain subsides and the doctor gives clearance, physical therapy begins. Initially, it focuses on gentle “restoring range of motion” to prevent stiffness (passive and active-assisted movements). As healing progresses, the emphasis shifts to “strengthening rotator cuff” muscles and other muscles surrounding the shoulder. This strengthening is vital for improving stability and “preventing re-injury.” Physical therapy also includes proprioceptive exercises, which help retrain the shoulder’s sense of position and movement.
- Gradual Return to Activity: The “recovery timeline varies” significantly from person to person. For a first-time dislocation in a younger, active individual, full recovery might take 3-6 months. For older individuals or those with recurrent dislocations, it could be longer. Return to sports or strenuous activities is gradual and guided by the physical therapist and doctor, ensuring the shoulder is strong and stable enough to prevent future dislocations. The goal is not just to get the shoulder back in, but to restore its full function and reduce the risk of future episodes.
Conclusion
Recognizing the signs of a dislocated shoulder is a vital skill that can empower us to take prompt action in an emergency. We’ve explored the “recap of key visual and sensory signs,” from the unmistakable squared-off contour and unnatural arm position to the excruciating pain, immobility, and potential numbness or tingling. We also differentiated between the common anterior dislocation and the less frequent, but equally significant, posterior and inferior types.
The most important takeaway is “emphasizing the importance of seeking professional medical help” immediately if a dislocation is suspected. Never attempt to reduce the shoulder yourself, as this can lead to severe and lasting damage. Medical professionals have the expertise, tools, and pain management strategies to safely diagnose and treat the injury, often confirming it with X-rays.
“The goal of treatment is to restore stability and function” to the affected joint. This involves careful reduction, a period of immobilization, and a dedicated course of physical therapy to strengthen the surrounding muscles and regain full range of motion. While the “long-term outlook” for most dislocated shoulders is positive with proper care, the risk of recurrence, especially in younger, active individuals, highlights the importance of thorough rehabilitation and adherence to medical advice. By understanding what a dislocated shoulder looks like and how to respond, we can contribute to better outcomes and help individuals on their path to recovery, ultimately “preventing future dislocations” through informed care and appropriate follow-up.


 Home
Home









