Introduction
The lining of the anus develops a small tear known as an anal fissure that typically causes bleeding and pain during bowel movements. Recent study findings indicate that chronic anal fissures may develop from benign conditions like constipation and could also be associated with colorectal or anal cancer. The article discusses the evaluation of anal fissures and designated methods through which oncologists can specify which cases require additional examination and treatment. The article shows important preventive steps and emphasises the need for immediate medical response.
Table of Contents
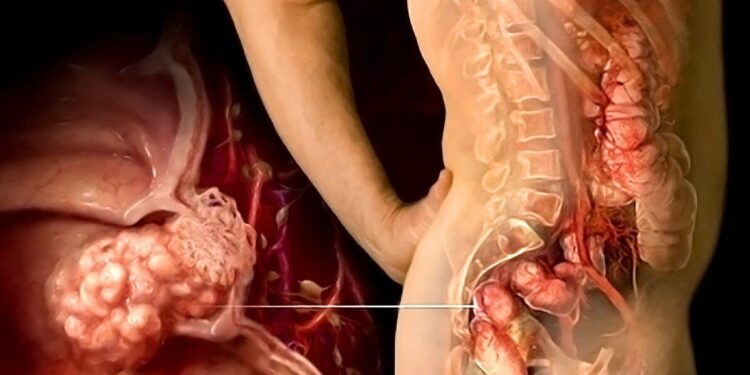
Understanding Anal Fissures
Anal canal trauma can be caused by factors like hard stools and persistent diarrhoea, along with childbirth and medical procedures that often lead to anal fissures. Proper care enables acute fissures to heal within a few weeks. When anal fissures persist beyond six weeks, they become chronic and raise concerns because they may indicate deeper health issues. Differentiating between acute and chronic anal fissures provides vital insight into long-term health outcomes and to know the potential risks involved.
Key Symptoms:
- Sharp pain during bowel movements
- Bleeding after bowel movements may appear on toilet paper or within the stool.
- Itching or irritation around the anus
- Chronic cases commonly present with a small lump appearing next to the fissure.
Patients with chronic conditions can develop extra symptoms such as a continuous anal spasm and a sentinel skin tag that make the clinical situation more complex.
The Connection Between Anal Fissures and Cancer
Anal fissures usually don’t represent severe medical conditions, but they might indicate anal or colon cancers if they remain persistent or fail to heal. Oncologists are particularly vigilant when fissures do not heal with standard treatment or are accompanied by unusual symptoms, such as:
- Persistent bleeding
- Significant weight loss
- Changes in bowel habits
- Unexplained fatigue
Further testing must be conducted by a medical professional to rule out cancer or other significant health risks when these symptoms appear. Continuous irritation or inflammation from untreated fissures can change the surrounding tissues, and the risk of cancer can increase over time, too.
Diagnostic Approach by Oncologists
Through a systematic evaluation process, oncologists identify possible malignancies in patients experiencing chronic anal fissures. The steps to evaluate the issue are stated below:
1. Medical History and Physical Examination
Oncologists begin with a detailed medical history, focusing on:
- Duration and frequency of anal fissures.
- The diagnostic process involves assessing related symptoms that show variations in bowel patterns along with bleeding tendencies.
- Family history of colorectal or anal cancer.
The physical examination requires a detailed visual inspection of the anal area to detect any abnormal masses and ulcerations as well as signs of chronic inflammation. Tough fissures with uneven edges may signal cancerous conditions.
2. Diagnostic Tests
To confirm or rule out malignancy, oncologists may recommend the following tests:
- Anoscopy or Proctoscopy: Medical professionals use Anoscopy or Proctoscopy techniques for direct examination of the anal canal in order to spot any irregular growths or lesions.
- Biopsy: In biopsy procedures, doctors obtain suspicious tissue samples to analyse them in labs for cancer detection.
- Imaging Studies: Specialists use combined CT scans and MRI and PET scans to study cancer progression within deep bodily tissues.
- Colonoscopy: Medical professionals perform a colonoscopy as an examination procedure on both the colon and rectum to detect polyps, tumors, and other abnormalities.
The extent of tissue damage is examined by doctors using imaging techniques, including endoscopic ultrasonography.
3. Laboratory Tests and Biomarkers
Cancer-diagnosing specialists perform blood tests to find cancer markers, including carcinoembryonic antigen (CEA). HPV infection tests allow medical professionals to detect anal cancer because they reveal substantial links between HPV infection and cancer development.
Treatment Strategies for Anal Fissures with Potential Cancer Risks
Management approaches for anal fissures require knowledge about their precise underlying cause. Oncologists collaborate with multidisciplinary teams to develop specific treatment plans once a cancer diagnosis or suspicion emerges. Medical diagnoses that are both prompt and precise allow physicians to determine appropriate treatment choices.
1. Management Without Surgery
Initial treatment for anal fissure concentrates on symptom relief and promotes healing:
- Dietary Modifications: Combining a high-fibre diet with more fluid intake results in having softer faeces.
- Topical Treatments: Calcium channel blockers with topical nitroglycerin ointments assist in lowering pain and improving blood flow to promote recovery.
- Injections of Botulinum Toxin: The use of Botulinum Toxin Injections causes fissures to close by lowering anal sphincter muscle tension and spasms.
Once cancer has been ruled out, medical specialists consider these treatments sufficient to address the issue. Conservative therapies address underlying conditions such as chronic diarrhoea and constipation to avoid more complications.
2. Surgical Procedures
Chronic fissures unresponsive to conservative treatments may require surgical intervention, such as:
- Lateral Internal Sphincterotomy: This procedure facilitates tissue recovery by lowering sphincter pressure.
- Fissurectomy: During this procedure, the surgeon removes the fissure along with surrounding scar tissues.
The primary goal of oncologists is cancer treatment immediately after its detection.
3. Cancer-Specific Treatments
- Radiation Therapy: It stands as the primary treatment method for anal cancer because it reduces tumors and relieves patient symptoms.
- Chemotherapy: Functions by enhancing radiation therapy effectiveness as well as attacking cancer cells on their own.
- Surgical Resection: The necessity of surgical resection arises in advanced disease because this procedure eliminates the diseased tissues or organs. Patients sometimes need highly invasive surgical interventions, such as abdominoperineal resection, depending on their medical situation.
When Should You See an Oncologist?
If standard treatments for anal fissures fail or worrisome symptoms develop, patients should pursue specialist consultation. Early meeting with an oncologist can be lifesaving, especially for patients with the risk factors mentioned below:
- History of HPV infection
- Immunosuppression (e.g., HIV/AIDS)
- Smoking
- Family history of colorectal or anal cancer
People with chronic fissures need regular check-ups from oncologists to identify any signs of developing cancer.
Preventive Measures and Lifestyle Changes
Preventing anal fissures and reducing cancer risk involves adopting healthy lifestyle habits:
- Dietary Fibre: A sufficient intake of dietary fibre reduces constipation, and this decrease in constipation helps prevent anal trauma.
- Regular Screening: Individuals older than fifty and those with inherited cancer risks require routine colonoscopies, which detect cancer at early stages.
- Avoid Straining: Proper toilet habits, along with limited sitting time on the toilet, help reduce anal pressure.
- Vaccination: People who receive the HPV vaccination have a lower risk of developing anal cancer.
Medical problems become less likely when individuals sustain healthy weights and steer clear of high-risk sexual practices. Long-term health depends on educating patients about preventive strategies.
Conclusion
Though anal fissures generally recover without treatment, medical intervention becomes essential to eliminate cancer as a possible diagnosis when the symptoms persist. An oncologist provides exceptional patient care through the combination of vital risk assessments and modern diagnostic technologies with individualised treatment plans. Prompt diagnosis and professional medical care reduce the risk of cancer and help in treating the anal fissures. Knowledge of risk factors combined with preventive actions leads to better health management and decreases the likelihood of anal fissures and cancer in the near future.


 Home
Home